MSC-100-IV (remestemcel-L) for the treatment of paediatric aGvHD is one of Mesoblast’s highest priority programmes. GvHD is caused when donor T-cells recognise host cells as foreign and attack them. It is a potentially severe and often fatal side effect of haematological stem cell transplants (HSCT, also called grafts), which are used to treat acute leukaemias and other types of cancer (Exhibit 2). There are two types of HSCT: allogeneic and autologous. Autologous (self) grafts do not cause GvHD, while allogeneic grafts use donor stem cells and can cause GvHD and therefore are potentially treatable with MSCs.
Exhibit 2: Haematological cancers and stem cell transplant types and use
Cancer type |
Comments |
Allogenic |
Autologous |
Acute myeloid leukaemia (AML) |
AML comprises cancerous myeloid cells, which normally produce innate immune cells, red blood cells and platelets. Patients who fail initial chemotherapy therapy have a poor prognosis. |
Yes, preferred treatment |
No |
Acute lymphocytic leukaemia (ALL) |
ALL is from cancerous leucocyte cells; these normally produce active immune cells. ALL is targeted by CD-19 CAR-T therapy. |
Yes, preferred treatment |
No |
Myelodysplastic syndrome (MDS) |
MDS is diagnosed due to anaemia and so tiredness as the marrow produces immature red cells. This progresses to AML in 30% of cases. |
Yes |
No |
Multiple myeloma (MM) |
MM is a cancer of mature B-cells (plasma cells that hinder the bone marrow from making normal blood and immune cells). May be treated by CAR T-cell therapies within a few years. |
Rare |
Main type of stem cell graft |
Lymphomas |
These are cancers of the immune system that have localised to the lymph nodes. Major subtypes now treatable with CD19 CAR T-cell therapies. |
Limited use |
Main type of stem cell graft |
Source: Edison Investment Research
GvHD occurs if there is a recognised HLA mismatch between the graft and host. GvHD can happen in even well-matched transplants as T-cells are highly sensitive to otherwise undetectable donor vs host differences. GvHD typically involves the skin (rash and dermatitis), liver (hepatitis and jaundice) and the digestive system (diarrhoea, abdominal pain). GvHD is most commonly managed with corticosteroids in first-line therapy and is often supplemented with low continuous immunosuppressive drugs as needed. The condition can be acute (aGvHD), involving a response within 100 days of transplant or a chronic response (cGvHD) that develops over several years.
aGvHD is graded on two common scales: the Glucksberg scale, which measures GvHD in the skin, liver and intestine and gives a composite score graded 0–IV, and the IBMTR scale (used in the Mesoblast trial), which is scored A–D and largely corresponds to Glucksberg. The prospect of patients with aGVHD depends on the severity.
■
Grades 0–I (Glucksberg) and A (IBMTR) are not clinically significant.
■
Patients with Grade II/B have skin or single organ involvement with an 80–85% chance or better of surviving more than one year.
■
Patients with Grade III/C have very severe disease involving usually the skin and other organs with about 30% chance of one-year survival.
■
Patients with Grade IV/D have more extensive GvHD than Grade III/C with a 2–3% chance of surviving one year.
The medical decision-making process for HSCT eligibility is multifaceted. Disease characteristics and patient characteristics (ie age, overall health, comorbidities, prior therapies and response to prior therapies) are thoroughly assessed to determine patient eligibility. Loose eligibility conditions for HSCT requires patients to be under 70 years of age (HSCT is rare over 70), be healthy and preferably have responded to first-line therapy. Nonetheless, the decision to proceed with HSCT remains a personalised medical opinion although success is elusive if such criteria are not met. A lot of the recent growth in allogeneic HSCT use is in patients aged over 60 who now account for about 30% of HSCT use compared to just a few percent in 2000. Moreover, there is an increasing trend in HSCT in patients over 70, which represented 4.6% of all allogenic transplants in 2016.
In the US, there has been overall strong growth in the use of HSCT to treat acute myeloid leukaemia (AML): there were 1,000 AML-related treatments in 2000 and about 3,400 in 2016. The linear growth pattern is about 150 new cases per year treated; this is not an exponential compound growth rate. AML is largely a disease of older adults (74.3% of patients are aged over 55 with 57.4% over 65). There is potential for further growth because there are 19,520 AML cases expected in 2018 in the US with 10,670 predicted deaths and 27% five-year survival. Expanding the market probably depends on significant progress in treating AML, a cancer type that has beaten all prospective new therapies to date. However, the AML age profile (the average age of first diagnosis is 68 years) also inherently means that fewer AML patients receive an HSCT.
Other cancers use HSCT less often; HSCT to treat acute lymphocytic leukaemia (ALL) is about 1,250 cases, about 50 new per year. This is a treatable cancer with chemotherapy: 68% five-year survival with 5,960 new cases and predicted 1,470 deaths in 2018.4 ALL is mostly (55.4%) paediatric (<20 years old). Hence, paediatric HSCT use for ALL is equal to AML whereas in adults, AML predominates. Refractory cases of ALL are now treatable with CD19 CAR T-cell therapies: Kymriah (Novartis) and Yescarta (Gilead) although numbers are still small, maybe 100–150 Kymriah uses in 2018. Use of a CAR therapy can enable a CR (88% of cases) and act as a bridge to an HSCT.
Myelodysplastic syndrome (MDS), a potential precursor to AML, is seen in about 1,000 HSCT patients in the US per year. There are also 1,000 cases in lymphoma and a few hundred cases in multiple myeloma; these cancers normally use autologous HSCT.
MSC-100-IV trial primary data success in Phase III
The primary endpoint of the Phase III trial was overall response rate at day 28 after dosing with 100m remestemcel-L cells or placebo given with corticosteroids. The endpoint includes both complete and partial responses. Patients received six infusions during the study. Infusions were administered twice weekly during the first two weeks (four in total), then once weekly over the following two weeks (two in total). Patients had either Grade C or D aGVHD involving the skin, liver and/or the GI tract, or they had Grade B aGVHD involving the liver and/or GI tract. Most patients (89%, 49/55) were grades C or D. CR was defined as resolution of aGVHD in all involved organs.
The overall response rate and CR rate were an impressive 69% and 29%, respectively. The 100-day survival data were also impressive: of the 38 patients who responded to the MSCs, 31 (87%) were alive at 100 days. In the 17 patients who did not respond at 28 days to MSCs, eight died (47%). The overall survival rate in all patients was 75%. These statistics emphasise the severity of the GvHD experienced by these children.
In September 2018, Mesoblast reported follow-up 180-day safety data. In patients who had a positive overall response to treatment with remestemcel-L at day 28, survival was 87% at day 100. At day 180, survival in patients who had an overall response at day 100 was 79% (p=0.001 by Kaplan-Meier survival estimates compared to non-responders). Overall day 180 survival for the entire remestemcel-L treated group was 69%. For comparison, a meta-review of 119 patients found 63% six-month survival after MSC use. Mesoblast notes the historical survival rates in patients with Grade C/D disease and failure to respond to steroids have been only 10–30%. The further Mesoblast data show response durability, a crucial competitive factor and important for reimbursement. The company announced in mid-April 2019 that the FDA has agreed to a rolling review of the BLA filing and initiated that rolling submission in May. Submission on a rolling basis allows Mesoblast to submit each module as it is completed, providing the opportunity for continuous communication between the two parties.
Market segmented by donors
The number of total grafts (adults and children) can be segmented by donor type in the US and Europe (Exhibit 3). Note that haploidentical grafts have very low aGvHD rates and are increasingly used if high-quality unrelated donors are not available; this is a marked new trend in the market. Cord blood donations are suitable for children, but their use has declined.
US 2016 CIBMTR3F data show about 8,500 allogeneic HSCTs for that year. In Europe, the European Group for Bone Marrow Transplantation reported that 17,641 patients received an allogeneic HSCT in 2016 (this includes data from 49 countries). These are then subdivided by donor type (Exhibit 3). Overall, US trends via CIBMTR data illustrate a sudden shift in 2013 towards haploidentical grafts from a low base (Exhibit 4).
Exhibit 3: HSCT by donor type, adult and paediatric in US and Europe 2016 data
Donor |
Notes |
US |
Europe |
Matched unrelated donors (MUD) |
Most (70%+) Caucasian patients can be found a match but other groups have fewer registered donors. If the HLA matching is stringent (10/10), the risk of GvHD is small. However, less precise matching often triggers GvHD. |
3,900 |
8,000 |
Matched related donors (MRD) |
Used when a sibling or another family member HLA match can be found. This is a preferred donor type if available. |
2,250 |
5,000 |
Cord blood |
Umbilical cord blood samples are frozen and can be used partly matched. They are used for hard-to-match patients. |
600 |
500 |
Haploidentical and other related mismatched donor |
This is a partly mismatched (two or more) graft from a related donor. They are used when no matched donor is available or if speed of transplant is crucial. The Baltimore protocol with post-transplant at cyclophosphamide reduces GvHD rates. |
1,750 (1,000 Haplo) |
2,500 |
Source: Edison Investment Research based on cited sources. Note: Cord blood is also used to treat genetic disorders. Market data CIBMTR (US) and EBMT (Europe).
Exhibit 4: US allogeneic stem cell transplants by donor type, all ages
|

|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org. Note: URD unrelated donor, HLA-iden sib Matched related sibling donor, URD unrelated matched donor, CB cord blood (about half are patients aged under 18. Other is mostly, but not entirely, mismatched related donor also known as haploidentical.
|
The main factors driving whether patients fall victim to GvHD is donor type and the degree of match. For instance, in a sample size of 8,041 patients, matched sibling donors (13.5%) demonstrated less risk of Grade III–IV aGvHD than unrelated donors (19.1%). On average, 17% of all patients sampled had Grade III–IV GvHD and paediatric rates (younger than 10 years of age) were 12.7%. Another review that evaluated matched unrelated donors between 2008 and 2012 found rates of about 30% Grade II–IV and about 12% Grade III–IV.
Other factors affecting GvHD include type of transplant (ie either bone marrow or peripheral cells) and type of prophylactic therapies. Intensive (myeloablative or MAC) conditioning, used before transplant to destroy the patient’s original immune system and residual cancer, leads to higher Grade III–IV aGvHD rates compared to reduced intensity conditioning.
As the number of patients undergoing allogeneic HSCT continues to increase and despite improved HLA matching and the expanding donor population, we expect the burden of aGvHD to rise correspondingly. Analysis of annual transplant activity between 2010 to 2015 in the US shows an increasing number of allogenic HSCT for several racial and ethnic groups with 16%, 43% and 20% increases for Caucasians, African Americans and other races, respectively. These data also revealed that trends in HSCT are affected by reimbursement decisions. To demonstrate, because Medicare agreed to fund HSCT transplants for MDS in 2010, the number of grafts for this indication in older adults increased substantially. Moreover, as similar funding will be provided for indications such as multiple myeloma and sickle cell anaemia in the coming years, it is expected that transplant numbers will similarly be affected.
Mesoblast’s MSC-100-IV for aGvHD is initially targeting paediatric patients. In children, there are about equal numbers of high-risk ALL and AML cases as well as rare inherited blood disorders treated with HSCT. Notably, research suggests children react more favourably to HSCT than adults. In the study published in 2018 analysing patient and donor characteristics for 1,815 paediatric patients who underwent HSCT from 1999 to 2011, it was noted the Grade III–IV aGvHD rate in children under the age of 10 was 12.7%, increased to 16.9% in children aged 10–19 and rose to 19% in adults.7 In another review, aGvHD reported registry rates in children were summarised according to donor type and degree of matching (Exhibit 5). There are 10 possible HLA genes in an individual, although some are less critical than others for compatibility. The minimum match is 6/6, but 8/8 matching is preferable. It is important to note, as with many GvHD review articles, the outcomes reported are variable and although the information is valuable, some of the data are considerably dated.
Exhibit 5: GvHD rates by donor type in paediatric cases
Door type |
Grade II only % |
Grade III–IV % |
Total Grade II–V % |
HLA identical sibling donor (10/10)‡ |
17 |
11 |
28 |
Unrelated matched donor (10/10)‡ |
32 |
8 |
40 |
Unrelated mismatched donor (6/6)‡ |
26 |
30 |
56 |
Cord blood high match‡ |
8 |
11 |
19 |
Cord blood low match‡ |
11 |
22 |
33 |
Haploidentical (MAC/RIC)* |
9/17 |
7/2 |
16/19 |
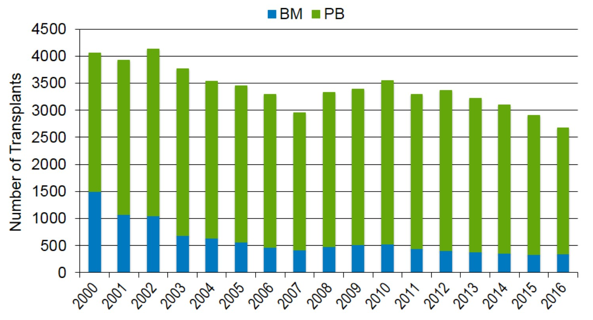
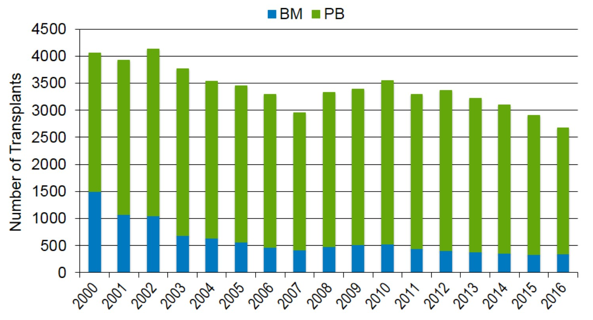
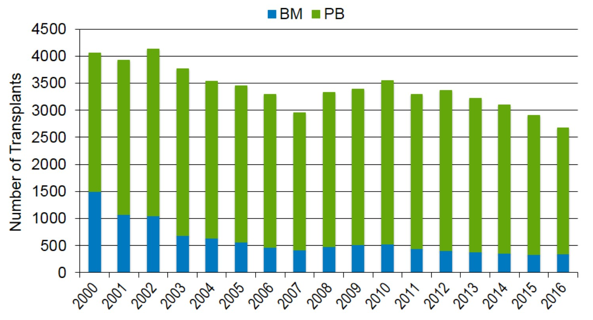
According to the CIBMTR, paediatric HSCT numbers were about 1,664 in 2016 (Exhibits 6 and 7). Unrelated matched donor (URD) HSCT surpassed the use of matched-sibling donor (MSD) over the last decade, which is likely due to the growing donor registry, improved HLA matching and comparable outcomes of related and matched unrelated donors. Trends appear to be stable for MSD transplants from 2012 onwards, whereas the use of cord blood, which peaked in 2009 at 48%, has since nearly halved. Overall, HSCT in children has remained relatively stable over the last decade.
Exhibit 6: HLA-matched sibling donor allogeneic HSCT in patients <18 years
|
Exhibit 7: Unrelated donor allogeneic HSCT in patients <18 years
|

|

|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org, PB = Peripheral Blood, BM = bone marrow
|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org, URD-CB = Cord blood from unrelated donor
|
Exhibit 6: HLA-matched sibling donor allogeneic HSCT in patients <18 years
|

|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org, PB = Peripheral Blood, BM = bone marrow
|
Exhibit 7: Unrelated donor allogeneic HSCT in patients <18 years
|

|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org, URD-CB = Cord blood from unrelated donor
|
According to the CIBMTR, adult HSCT numbers were about 6,900 in 2016 (Exhibits 8 and 9). Similar to paediatric HSCTs, adult URD HSCT quickly surpassed the use of MSD between 2007 and 2013, which then levelled between 2013 and 2016. Notably, the number of allogenic HSCT for malignancies continues to increase patients older than 60 years of age and even over the age of 70. We expect this trend to continue along with the rise in HSCT use among the aging population.
Exhibit 8: HLA-matched sibling donor allogeneic HSCT in patients ≥18 years
|
Exhibit 9: Unrelated donor allogeneic HSCT in patients ≥18 years
|
|

|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org, PB = Peripheral Blood, BM = bone marrow
|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org, URD-CB = Cord blood from unrelated donor
|
Exhibit 8: HLA-matched sibling donor allogeneic HSCT in patients ≥18 years
|
|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org, PB = Peripheral Blood, BM = bone marrow
|
Exhibit 9: Unrelated donor allogeneic HSCT in patients ≥18 years
|

|
Source: D'Souza A, Fretham C. Current Uses and Outcomes of Hematopoietic Cell Transplantation (HSCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org, URD-CB = Cord blood from unrelated donor
|
US HSCT trends mirrored in Europe
European allogeneic HSCT trends in both paediatrics and adults are strikingly similar to US patterns. According to EBMT,6 allogenic HSCT continues to rise at about 2% per year, whereas some indications continue to increase and others have fallen. In 2016, approximately 38%, 16%, 11% and 8% of all allogeneic HSCT were attributed to AML, ALL, myelodyplastic/myeloproliverative neoplasm (MDS/MPN) and non-Hodgkin lymphoma (NHL), respectively. Compared to the year prior, there were increases in HSCT for ALL, MPN and severe aplastic anaemia (a bone marrow failure disorder) by 6.3%, 21.4% and 13.4%, respectively. Notably, the total number of paediatric (18 years and younger) allogeneic grafts increased by 6.2% in comparison to 2015.
Since 2011, the use of cord blood has decreased dramatically, whereas haploidentical HSCT has continued to increase. In contrast to US trends where we see an increase in URD, such grafts in Europe appear to have levelled between 2015 and 2016 whereas the use of MSDs increased. Interestingly, further analysis showed the majority of URD HSCT were performed in high-income countries whereas less wealthy countries used haploidentical HSCT more often, which eludes to the fact that economics may influence donor choices and, consequently, outcomes.
Mesoblast’s remestemcel-L will be FDA fast tracked and potentially approved in the US in H120. However, there are other therapies being investigated for the treatment of aGvHD. JAK inhibitors are the biggest challenge for Mesoblast’s remestemcel-L to overcome with ruxolitinib (Jakafi) recently being approved by the FDA for steroid-refractory aGvHD in May 2019.
Exhibit 10: Current and recent late-stage GvHD trials with 28-day steroid refractory responses
Interventions |
Trial reference and sponsor |
Patients |
Data due |
Comments |
Overall response |
CR |
Therakosa Cellexa |
NCT02524847 Mallinckrodt |
48 |
January 2022 |
Paediatric patients with steroid refractory aGvHD. The extracorporeal system ablates white cells using Uvadex (Methoxsalen) a photosensitiser. It is approved for palliative treatment of cutaneous T-cell lymphoma. |
|
|
Itacitinib |
NCT03139604 (Incyte) |
436 |
H219 |
A selective JAK1 inhibitor in a placebo-controlled study (GRAVITAS-301) for aGvHD in combination with steroids. The endpoint is day 28 response. There are reports of long-lasting remissions. It has EU orphan designation. |
64.7% |
|
remestemcel-L |
NCT02336230 Mesoblast |
55 |
Reported |
Trial in paediatric steroid refractory GvHD using human MSC. Day 28 responses. Fast track granted. Rolling submission initiated in May 2019. |
69% |
29% |
Ruxolitinib (Jakafi) |
NCT02953678 InCyte |
71 |
Reported |
Jakafi (Incyte, US) and Jakavi (Novartis, ex-US) is a JAK 1/2 kinase inhibitor recently approved for steroid refractory acute GvHD in patients over the age of 12 and is also approved for the rare blood cancers myelofibrosis and polycythemia vera. There were side effects in many patients. |
57% |
31% |
NCT02913261 Novartis |
308 |
June 2019 |
REACH2 study for EU registration. Randomised open label study with a day 28 response endpoint. It had an ORR of 85.4% for cGVHD. |
N/A |
N/A |
T-Guard |
NCT02027805, Xenikos |
30 |
Reported |
Phase II data, 20 patients, a dual monoclonal antibody against CD3 and CD7 to deliver an immunotoxin (possibly ricin) to kill T-cells and NK cells. |
60% (180-day survival) |
50% |
Source: Edison Investment Research based on Clinicaltrials.gov data and company websites
The primary endpoint for ruxolitinib was response rate at 28 days. In the US, the REACH1 trial for a supplemental NDA filing (as already approved for cancer) reported a 57% overall response rate and a 31% CR rate, although this was heavily skewed by an outsized effect in moderate Grade II patients who had an 82.6% response rate (Grade III patients had a 41.2% response rate and Grade IV patients had a 42.9% response rate). In contrast, remestemcel-L appeared to have a stronger impact on more severe patients, with a 73% response rate in Grade D patients, 70% in Grade C and 50% in Grade B (note Grades B–D are roughly equivalent to Grades II–IV with higher letters/numbers indicating increased severity. Side effects for ruxolitinib included anaemia (75%), thrombocytopenia (75%), neutropenia (58%), infections (55%) and oedema (51%), making it a relatively toxic drug. There can also be complications associated with viral infection and the toxicity profile is a significant limiting factor of ruxolitinib in children. Moreover, the drug dose needs to be reduced in patients with impaired liver function if they have reduced platelet levels. This may complicate or potentially rule out dosing in GvHD patients who have liver involvement, although we do not have data on this.
Frequency of aGvHD varies roughly between 30% and 80% depending on several factors including type of transplantation. To forecast both paediatric and adult numbers in the US and Europe, we assume a 40:60 split between MSD and URD, respectively, as we see a trend decline in cord blood use in children. We have used CIBMTR data as the basis for our US forecasts then increased the numbers by about 10% to include Canada. Likewise, we use EBMT data from 49 countries as the basis for our European forecasts, where we assume stable URD use and increases in MSD.
In an effort to maintain robust estimates, we assume 39% and 59% probabilities of developing Grade II–IV aGvHD, whereas the likelihood of developing aGvHD is less likely from an MSD, than an URD in both children and adults. We further calculate frequencies of Grade II aGvHD presenting with skin plus other organ involvement and Grade III–IV aGvHD as proportions of all possible Grade II–IV cases (Exhibit 11). What is more, resistance to first-line steroid treatment is also highly variable with reported refractory rates of 30% to 60%.12 We use 44% as an overall figure for steroid-refractory cases in aGvHD.
Exhibit 11: aGvHD market assumptions
|
MSD |
URD |
Grade II–IV |
39% |
59% |
Grade II (Skin plus other organ involvement) |
34% |
15% |
Grade III–IV |
40% |
54% |
Source: Edison Investment Research. Notes: Most patients in Mesoblast’s trial were Grade III–IV, or Grade II with skin plus other organ involvement.
The specific indication for remestemcel-L validated in the recent Mesoblast trial is paediatric patients who have steroid refractory aGvHD Grades B–D after a stem cell transplant. Based on these assumptions, we expect 396 possible paediatric cases in North America, which translates to approximately 257 treatments per year if we apply 65% share as we expect it to be the treatment of choice because it is less toxic than the JAK inhibitor competitors and appears more efficacious in more severe patients. It will also be the only therapy where children below the age of 12 will be on the label. We assume a launch price of US$285,000, which is around a 40–50% premium to Temcell pricing in Japan. Moreover, we assume direct US marketing by Mesoblast and thus include a simple estimate for direct sales costs of US$5m per year. There are relatively few centres for stem cell transplant (c 170), so sales and technical support should be simple to organise with a small team. Mesoblast already manufactures using Lonza. We assign an 80% probability of success to the North American paediatric indication following excellent 180-day data and assume an H120 launch after the rolling submission was initiated in May. We assign a lower probability of success for adult use as no trials are known; we assume some off-label use. We also assume adult market penetration is lower.
In Europe, we estimate 1,325 possible paediatric cases in accessible counties, which translates to about 582 treatments per year if we apply 50% share. Europe is assumed to be accessed through a marketing partner, with Mesoblast taking 60% of revenues and supplying product. All European Medicines Agency reviews take 210 days (excluding clock stops at 120 and 190 days). If an approval recommendation is made, there is a further period (about 90 days) before formal approval. There then needs to be country-by-country price negotiations, which can be prolonged. Europe is a price-sensitive market so we assume a launch price at a 30% discount to North American pricing. We also assume lower market shares, but note that Europe carries out over twice the number of stem cell transplants (Germany being key) as the US so the market is worthwhile. Mesoblast has not given any timelines for EU filing. We assume sales from FY22. Furthermore, MSCs are already used in some cases to control GvHD in Europe. According to the 2016 European Society for Blood and marrow transplant activity survey, 421 uses of MSCs for GvHD were reported, but these figures are not broken down by age.6
The much larger market is adult use. Mesoblast has not run trials in adults so this indication depends on gaining a label extension, which may require further adult trials. In Europe, this might be a conditional approval, which is a full approval requiring further data and a subsequent review; Zalmoxis was EMA approved on this basis. There was a 244-patient, Phase III randomised, placebo-controlled study run by Osiris (before the product was acquired by Mesoblast in 2013). Data were released in 2009 but the trial failed to meet the primary endpoint, although there was a response in adult subgroups with liver (p<0.05) and gut (p<0.05) involvement and the paediatric subset. Of the 75 children with acute, severe, multi-line refractory GVHD, 61% responded to Prochymal and 76% of these were alive at day 100. If adults are included, either on an expanded label or by off-label use (assuming reimbursement), then on the same basis with an expected 45% and 25% market share in North America and in Europe, respectively, Mesoblast may gain 1,660 adult North American patients and 2,265 additional European adult patients.
Exhibit 12: aGvHD market forecast
Territory |
Class |
Cases |
Probability of success |
Max share |
Peak sales (US$m2028) |
North America |
Paediatric |
396 |
80% |
65% |
$103.2 |
|
Adult |
1,662 |
55% |
45% |
$300.0 |
|
|
|
|
|
|
EU |
Paediatric |
1,324 |
70% |
50% |
$58.1 |
|
Adult |
2,266 |
50% |
25% |
$113.0 |
Japan |
All allogeneic |
3,600 |
100% |
N/A |
N/A |
Source: Edison Investment Research
There is also potential use in cGvHD, a major issue where the prevalence of cases is up to 50%. At this time, there are no announced trial plans for adult use and we assume further studies will be required to show efficacy, establish doses and gain reimbursement. EMA filing timelines have not been confirmed by Mesoblast.
Note in terms of pricing economics that as most Grade C or D patients die within 12 months (see above), getting a CR in about 30% of paediatric patients will be highly cost effective. The 180-day survival data are encouraging. Such patients have already had a US$350,000–800,000 stem cell transplant after cancer therapy. We expect a more detailed pharmaco-economic analysis to be published once response duration data are accumulated.
End-stage HF, NYHA Class IV
According to UNOS, there were 3,408 heart transplants in the US in 2018. About 40–50% of these used an LVAD as a ‘bridge to transplant’ (BTT). LVADs may also be used as ‘destination therapy’ (DT) if a patient is unsuitable for a transplant and would otherwise die. This use is formally off label in the US but allowed in the EU. Sales of LVAD devices in the US are hard to assess, as the leading companies have been acquired. Based on an analysis of utilization data from the Agency for Healthcare Research and Quality (AHRQ), approximately 4,500 circulatory assist devices are implanted annually in the US.
In December 2017, the FDA granted Mesoblast a Regenerative Medicine Advanced Therapy designation for MPC therapy to treat patients with left ventricular systolic dysfunction and an LVAD. Hence, a successful outcome after FDA discussions could lead to a US approval and marketing, although further studies may be required. A result in Class IV patients would indicate tissue re-modelling to gain function and could be a positive sign for the Class II–III patient study.
In a small 30-patient Phase II randomised study, 25m MPC (fewer than the 150m cells used currently) were injected into the patient’s heart at the time of LVAD insertion. Of 20 treated patients, 10 (50%) had a 30 minute or better wean at 90 days, whereas only 20% of 10 control patients could be weaned off the LVAD; this was not statistically significant (p=0.24) due to the trial size. However, further analysis indicated a 93% probability that MPCs had an effect with longer wean times. There were no safety issues. There was no difference in ejection fraction (percentage of blood in the filled left ventricle expelled from the heart during contraction, or systole): 24% vs 22.5, or in the six-minute walk test distance. After one year, 40% of MPC and 30% of placebo patients were weaned off their LVAD. The data also demonstrated that the MPC group had a significantly longer time to first major GI bleeding event (p<0.05) versus the sham comparator.
The US National Heart, Lung and Blood Institute has run, funded and consequently controlled a 159-patient trial of Revascor in end-stage HF patients who are having an LVAD implanted. The experimental arm of the trial includes the injection of 150m MPC cells into the heart muscle during the open-heart implant surgery versus a sham control solution. An LVAD7F is a small implanted pump powered by an external cable used to support blood flow in patients where the left ventricle is so distended it cannot pump enough oxygenated blood to meet the body’s resting demand. It pushes blood from a hole bored into the base of the heart’s left ventricle to the aorta (the main artery). LVADs can be used for many years, but they are ideally temporary.
Six-month data from the Phase IIb trial were presented in a late-breaking session at the American Heart Association Scientific Sessions on 11 November 2018. The primary endpoint of temporary weaning from full LVAD support was missed (p=0.55), whereas the average proportion of successful temporary weans was 61% and 58% in the MPC and sham groups, respectively. According to the company, this was likely attributable to the high rate of pump thrombosis, which is a device malfunction that consequently reduced the number of possible wean attempts as well as the heterogeneous nature of study population that included patients with ischemic and non-ischemic HF with LVADs for either BTT or DT. Post-hoc analysis revealed that temporary weaning was achieved in the more brittle, ischemic HF patient sub-group, which represents 44% of the total trial population (p=0.02).
Nevertheless, the company highlighted that there was a significant reduction in major GI bleeding events (Exhibit 13) in the MPC group versus control (p=0.02), which supports feedback from the June 2018 FDA Type B meeting. The FDA concluded that reduction of non-surgical GI bleeding is an unmet clinical need for patients with LVADs, while temporary wean is considered a biomarker and is not necessarily a clinically meaningful outcome.
Exhibit 13: Cumulative incidence of major GI bleeding events
|

|
|
|
Moreover, mortality rates (14% vs 15%) and overall time to transplant were similar between the two groups despite a non-significant increase in allosensitisation to HLA Class I antibodies in the MPC group (26% compared to 9% controls). Mesoblast did not comment on several secondary outcome measures including physiologic assessments and histopathological assessments of myocardial tissue that may elude to the future success of the larger CHF indication. Mesoblast recently met with the FDA and the agency provided guidance to the company for the pathway to approval for the LVAD indication. Importantly, the FDA reiterated that a reduction in major mucosal bleeding events is an important outcome for patients and that a reduction in those events can serve as the primary endpoint in a confirmatory Phase III trial. Secondary endpoints would include various parameters of cardiovascular function.
We include the LVAD indication in the Revascor CHF value estimate and assume that Mesoblast markets directly. If the larger CHF indication is approved, the sales may shift to a new marketing partner.
The main HF study, DREAM HF-1, is for the efficacy and safety of Revascor for HF. The Phase II data set published in 2015 provides supportive data for the Phase III 150m MPC dose.
The Phase II had three dose levels and enrolled 60 New York Heart Association (NYHA) CHF Class II and III patients. This included 20 patients per dose level: 15 patients plus five mock injection controls. It was single blind, so patients did not know which treatment they received (MPC or sham) but physicians did. Doses were 25, 75 and 150m MPC injected into the heart via a catheter. The Phase II was conducted using cells from only one donor.
On the original endpoint, based on revascularisation (ie cardiac death, coronary revascularisation and non-fatal heart attack), there was no effect.11 However, the Phase II analysis used a post-hoc HF major adverse cardiac event (MACE) endpoint as it was felt to be more relevant to a paracrine MPC action. HF-MACE events relate to heart functionality factors that may be influenced by MPC if they enable heart muscle remodelling and repair. Most events were decompensated HF, which is caused when the heart fails to maintain enough blood supply and is diagnosed by increased breathlessness, fatigue and fluid retention. On the formal primary endpoint, there were five 150m dose events vs five control events, but these were affected by other cardiovascular patient complications such as old, failing vein grafts. Crucially, the 150m MPC dose patient group had no HF-MACE events, which demonstrated statistical significance compared to controls (p=0.025). Mesoblast also notes that 11 patients with left ventricle end systolic volume (LVESV, or the volume of blood left in the heart after it has fully contracted) of more than 100mL (normally about 50mL) responded better to a 150m MPC dose. There was no difference in the ejection fraction (EF): 34% baseline, 31% after 12 months. There were no long-term improvements in NYHA class and a trend (not significant) in the six-minute walk test. However, this was a small study.
The triple-blinded DREAM HF-1 trial completed recruitment of 566 patients with NYHA Class II–III HF on stable medication across 55 centres in North America. The primary endpoint is ‘time to non-fatal recurrent decompensated HF events’. The trial has been through design changes, in particular a reduction in size from 1,730 to 1,165 in 2014 to the current ~600 in 2016 due to a change in the statistical plan and primary endpoint. Teva withdrew from the partnership in mid-2016 due to a change in strategic direction according to Mesoblast as the company focused more on generics rather than innovative drugs. Mesoblast has funded the trial since then, thus providing greater profit potential upon approval. All interim futility checks have passed the specified criteria (undisclosed). In February 2019, Mesoblast announced the last patient has been dosed and the trial will complete when adequate primary endpoints are collected. Results are expected in H120.
If there is a positive outcome, a further Phase III may be required by the FDA unless a regenerative medicine advanced therapy (RMAT) designation is granted. Entresto (see below) was approved in the same target population after a single, large study. Any further study, if needed, is likely to take at least three years to recruit, with a year to the final read out.
An EMA filing is expected; the EMA has given approval on a conditional basis to the cell therapy Zalmoxis on limited data. However, European pricing discussions and reimbursement can take several years to be agreed. Mesoblast has not given any EU guidance as we assume a US approval is the priority.
In our July 2016 note, we estimated a 2023 launch date with a further study. We recognise that this could be earlier, but it could also be much later as any second trial is not likely to complete before 2023–2024, implying a 2026 launch. Consequently, we have left the current assumption unchanged at 2023.
Many generic, small-molecule treatments alleviate the symptoms of HF and control blood pressure, but do not cure the condition. The major change in the guidelines for managing congestive HF since 2013 (US and EU) is in the use of Entresto (Novartis, a combination of valsartan (an angiotensin receptor inhibitor) with sacubitril (a neprilysin inhibitor).
Entresto is used to treat chronic NYHA Class II–III patients with reduced EF who are using an angiotensin (ACE) inhibitor or angiotensin receptor-blocker. Entresto sales have been slow to develop since the mid-2015 launch, but in 2018 Novartis reported US$1bn in sales, up 102% on a constant currency basis year-on-year. The price is at least US$4,500 per year, depending on the source. Entresto reduces the hazard ratio of hospitalisation to 0.8 and of death to 0.79 relative to the ACE inhibitor enalapril.
There are also some small cardiac cell-based trials running, however, these are from small companies. Capricor ran a Phase I MPC study with good results but is not developing the indication. CardioCel reported good Phase II data in 22 patients in a two-arm cross-over design seeing LVEDV and LVESV reductions and six-minute walk test gains. US StemCell has a small cardiac muscle trial running. Celyad (then Cardio3) abandoned its C-cure cardiac progenitor cell therapy after missing the primary endpoint in a Phase III study. There are also some academic cardiac studies.
CHF market for stem cells
Entresto is a twice-daily tablet, whereas direct cardiac injection of 150m MPCs is a one-off invasive procedure requiring a specialist catheter facility. Use of MPC therapy will be concentrated in those who do not respond adequately to Entresto and who may be undergoing a catheter procedure anyway. The payer cost for the MPC therapy will be boosted by the catheterisation procedure. Uptake will also depend on Medicare allowing these additional costs to be fully reimbursed; these negotiations can be protracted but again this depends on the strength of the Phase III data.
We have taken as a proxy those patients with HF with a reduced ejection fraction <40% and NYHA Class III symptoms and estimate that 726,000 patients may be prime candidates for Revascor treatment (Exhibit 14). We have thus increased uptake into this proxy population to 5.0% in both the US and in Europe (previously 2.5% in the US and 2% in Europe), as we have a more focused representation of the prime candidates for treatment.
Exhibit 14: Candidates for Revascor therapy
|
% of HF patients |
Number of US HF patients |
Notes |
US HF patients |
|
6,050,000 |
Based on American Heart Association estimate of 5.7m in 2012, escalated at 1.5% per year. |
LVEF < 40% |
48 |
|
Fonarow et al 2011a, citing ADHERE, GWTG-HF, OPTIMIZE-HF, Olmsted County studies. |
Percent with NYHA Class III |
25 |
|
Average percent in NYHA Class III–IV among patients with LVEF<35% or <40% in: ADVANCENT registryb (27.5%); Improve HF registryc (24.6%); and according to the National Heart, Lung, and Blood Institute estimates of patients with NYHA Class III is 25%. |
Prime candidates for MPC-100-IM therapy (LVEF <40% +Class III HF) |
12 |
726,000 |
|
Patients treated at 5.0% uptake of eligible patients |
1 |
36,299 |
|
Source: Edison Investment Research. Notes: aFonarow et al. Am Heart J 2011;161:1024-1030; bHanna et al. J Am Coll Cardiol 2006;47:1683-8; cFonarow et al. Circulation. 2010;122:585-596.
Due to the more focused addressable population and comparable biologic therapies, we now assume Revascor is priced at US$50,000 (previously US$20,000) per treatment per year in the US and US$20,000 per treatment in Europe (previously US$15,000). However, we caution that the price and reimbursement level is highly dependent on the data from the pivotal trial and the cost-benefit analysis of treatment (ie if this therapy can save money by reducing time in hospitals). Our Class II–III CHF forecast before probability adjustment assumes US$2.2bn in peak US sales. We forecast a further US$1.0bn in European revenues.
MPC-06-IDH: Chronic lower back pain
The spinal vertebrae are separated and cushioned by intervertebral discs of connective tissue made and maintained by mesenchymal cells. Disc degeneration or injury can cause chronic back pain.1 In February 2014, Mesoblast reported the results of using a single MPC intradisc injection. This was a 100-patient, four-arm Phase II trial in chronic moderate-to-severe discogenic lower back pain. The results were clear, signifying this indication is very promising.
The current Phase III trial in 404 patients initiated in 2015 and was fully enrolled at the end of March 2018. There is a two-year endpoint, so the primary outcome should be announced in Q220. The trial includes three arms: rexlemestrocel-L alone, rexlemestrocel-L combined with hyaluronic acid (a dense natural gel), or placebo (saline). The primary endpoint is a composite of three measures:
■
Lower back pain. In Phase II, 59.3% of the patients who received the 6m cell dose had a 50% or better reduction in pain, which is measured using a visual analogue score, compared to 12.5% of placebo patients (p=0.023).
■
Improvement on the Oswestry Disability Index (ODI). The ODI is self-scored from 1–5 in 10 sections and the score is then doubled so it is out of 100.6F A 15-point gain is regarded as clinically meaningful and the index is subjective. In the Phase II, 50% of patients who received the 6m MPC dose showed an improvement compared to 17.5% on placebo, p=0.05.
■
No post-treatment interventions with two years. By 12 months, 25% of patients in the saline control group had an additional intervention compared to 6.9% of MPC-06-ID patients.
In the Phase II, on this composite endpoint, the MPC-06-ID group showed 44.4% response compared to 11.8% on placebo (p<0.05). This is an excellent basis for Phase III.
In September, Mesoblast announced a licensing agreement with Grϋnenthal to develop and commercialise MPC-06-ID in Europe and Latin America. As part of this agreement, Mesoblast will receive milestone payments that could exceed US$1bn, including US$15m on signing, US$20m on receiving regulatory approval to begin a confirmatory Phase III in Europe and $10m for other clinical and manufacturing outcomes expected in the next 12 months (US$45m in total in the first year of the agreement). Mesoblast will also receive tiered double-digit royalties on sales. Importantly, Mesoblast retains the rights for key markets such as the US and Japan.
A 2009 study found a US chronic back pain prevalence of over 10% that was rising rapidly due to population aging, sedentary lifestyles and obesity, which equates to over 30 million Americans. There are no systematic US population surveys, so larger estimates need to be treated cautiously. Medical use surveys show 52 million doctor or hospital visits in the US in 2010 due to lower back pain in the US. In 2011, there were 369,900 operations on vertebral discs and over 1 million spinal operations according to a US survey.
Pharmaceutical options managing the chronic back pain symptoms include pain relief analgesics, anti-inflammatory agents, or epidural steroid injections. About 15%, or 4.5 million, of patients do not respond to these. Therefore, there is a large potential market for a new non-surgical therapy. About 10% of the patients who fail to respond undergo surgical interventions such as spine fusion, discectomy or artificial disc insertion. These are not necessarily effective. There are gel products to inject into the disc as long as the disc capsule is intact; these can relieve pain for up to 18 months.
As responses to current therapies and surgery are poor, this indication could serve a large market. Administration of the product, although not simple, can be done as an outpatient procedure by a physician who will earn a fee, aiding acceptance. It is an ideal indication for an allogeneic product.
Our current market forecast has increased to account for the change in price and is primarily attributable to comparable biologic therapies. We now use a price of US$10,000 (previously US$5,000) and a peak US market penetration of about 200,000 doses plus about 155,000 in Europe (at US$7,500 in Europe, previously US$3,750). Mesoblast is assumed to have a marketing partner for both geographies. We assign the project a 50% probability of success.